How the AMA secretly sets prices for health care in the US.
How the AMA secretly sets prices for health care in the US.
The Specialty Society Relative Value Scale Update Committee (or RUC, pronounced “ruck”) is a committee of the American Medical Association (AMA) that meets in secret to divvy up roughly $85 billion in U.S. taxpayer money every year. Of course that's just to get started. Because of the way the system is set up, the "values" the RUC comes up with wind up shaping the very structure of the U.S. health care sector, creating the perverse financial incentives that dictate how U.S. doctors behave, and affecting the annual expenditure of nearly one-fifth of the United State's GDP, $2.7 trillion dollars.
Is there anyone who really thinks that this is a good system?
From this article from Washington Monthly
While these doctors always discuss the “value” of each procedure in terms of the amount of time, work, and overhead required of them to perform it, the implication of that “value” is not lost on anyone in the room: they are, essentially, haggling over what their own salaries should be. “No one ever says the word ‘price,’ ” a doctor on the committee told me after the April meeting. “But yeah, everyone knows we’re talking about money.”
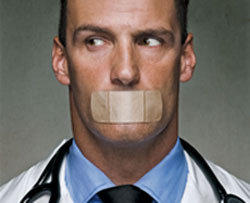
That doctor spoke to me on condition of anonymity in part because all the committee members, as well as more than a hundred or so of their advisers and consultants, are required before each meeting to sign what was described to me as a “draconian” nondisclosure agreement. They are not allowed to talk about the specifics of what is discussed, and they are not allowed to remove any of the literature handed out behind those double doors. Neither the minutes nor the surveys they use to arrive at their decisions are ever published, and the meetings, which last about five days each time, are always closed to both the public and the press. After that meeting in April, there was not so much as a single headline, not in any major newspaper, not even on the wonkiest of the TV shows, announcing that it had taken place at all.
In a free market society, there’s a name for this kind of thing—for when a roomful of professionals from the same trade meet behind closed doors to agree on how much their services should be worth. It’s called price-fixing. And in any other industry, it’s illegal—grounds for a federal investigation into antitrust abuse, at the least.
and this about why the AMA want's to control this:
The first boon is that, in order to be on the RUC, specialty societies must become dues-paying members. At a time when the AMA has struggled against being overshadowed by specialty societies, controlling the RUC prevents what might otherwise be a rapid exodus of membership. As one RUC member told me bluntly, “No one cares about AMA. They care about the RUC.” And that’s a lucky break for the AMA. In 2012, dues collection actually increased by 3 percent, topping out at $38.6 million for the year. Cha-ching.
The second boon for the AMA is that by controlling the RUC, it controls much of the source code that our health care system uses to operate. Every single one of those roughly 9,000 medical services and procedures has its own five-digit code, known as current procedural terminology (CPT), and the AMA owns them all. That means that anyone—physicians, labs, hospitals, you name it—who wants to bill Medicare, Medicaid, or a private insurance company has to purchase either AMA books and products, or products from other software companies that pay AMA royalties and licensing fees to use the CPT codes. According to its annual report, in 2012 the AMA made $83.1 million in “royalties and credentialing products,” a large chunk of which comes from licensing CPT. Again: cha-ching.
And that’s just the monetary stuff. The third boon—the real power curve—is the fact that the AMA’s control of the RUC makes it indispensible to everyone and everything in a $2.7 trillion health care industry. That includes specialty societies, primary care organizations, and medical device and pharmaceutical companies—all of whom have something big to gain or lose from the RUC’s decisions.
Snide and snarky comments welcome in moderation if you're in the US. Better ideas from outside of the US even more welcome.